Individuals with ostomies can have a slight fear of not being able to handle the pouching system correctly and in result cause complications. A stoma can be placed in many different ways and the placement could potentially determine how one should care for it.
Pre-cut pouching systems allow for a range of proper care from a flange opening of 3/4 inches (19mm), 1/8 of an inch (3-4mm) to 1 and 3/4ths of an inch (44mm) or even possibly a 2 inch (51mm) opening. These increments are set a little bit larger than the average stoma placement in order to fit around it properly. If the opening of the flange happens to be the same size of your stoma, this could cause issues and trauma to the stoma. If your stoma is in a convex flange placement, the pre-cut pouch being a bit larger matters quite a bit. A convexed flange tends to be a bit firmer than the flatter counterpart which requires a little more wiggle room. It is extremely important to understand that not all stoma pouches come in a pre-cut option, so if a pre-cut is what you desire than consider switching different name brands.
If a certain brand does not have the pre-cut option then it is possible to cut the flange carefully with flange cutters. These specialty designed scissors are cylindrical metal devices with a sharp blade-like edge that are made to cut swiftly through the flange. Flange cutters are available in round and oval shapes to make the process a bit more easier. When using flange cutters it is to be noted that flanges should be cut on a solid surface to prevent any damages to the surface beneath it.
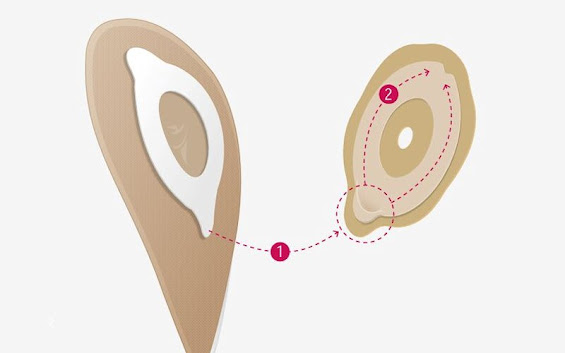
Newly designed technology called CMT, or ConvaTec Moldable Technology, is another option when it comes to ostomy care. This technology is designed using a special pliable technology that allows you to form the opening of the flange to the desired shape and size needed. In order to use this product you will do the following:
Using your fingers, carefully roll the inner edge of the flange outwards until it meets the desired shape and size needed.
Once firmly applied, the rolled edge will unravel until it touches your stoma.
Once the edge meets the stoma, it will form a soft cuff around the stoma.
This cuff will expand and shrink during normal function due to its elasticity.
The benefits of this new, upcoming technology is that unlike most traditional barriers, the worry of the barrier coming into contact with your stoma is gone. The logic behind this is that the technology has been designed to dismiss any trauma to the stoma itself. However, this product has been mainly designed for protruding stomas only. If the stoma is not raised then there is no barrier preventing the rolled edge from unraveling and uncovering the stoma. The ConvaTec Moldable Technology comes in a two piece system and for some ostomy patients can be a hassle if they are desiring a one piece application.